The Evidence-Based Clinician versus the Individual-Based Clinician
By Jay Dicharry, MPT, SCS
1. Introduction
We hear time and time again:
Are you an evidence-based clinician?
You know what?
Your patients don’t care.
There’s a patient in front of you in your treatment room right now. She is incredibly frustrated – and possibly even a bit scared – of what she’s dealing with, how this impacts her individual identity and running goals she set for herself this season. And she just wants to get BETTER!
2. Evidence-based medicine
The body of literature around running has progressed significantly over the past two decades, and sharply within the past 5 years. And you consider yourself a savvy evidence-based clinician. You have Google Scholar alerts set up for new articles and scour Pubmed weekly. And you have the best intentions to apply these cutting-edge findings to the patient in front of you.
However, the individual in front of you may not respond exactly the way we intended them to based on a study looking at an average response in a specific group of people. Why? Well, your patient likely isn’t in that exact group! The paper you read highlighted the outcomes of an intervention in a cohort of sedentary college-age students. Or maybe the paper assessed a novel treatment in a group of elites runners. But the patient who came to you for help is not at all similar to the subjects in those studies. She’s a competitive masters-age runner with a significant number of injuries under her belt from the last 25 years of training.
Research is quite powerful. It shows us the result of interventions in controlled environments so we can identify what’s successful, and what’s not. Unfortunately, your patient likely doesn’t live in a controlled research setting. To minimize confounding variables, the inclusion criteria for the studies in the back of your brain featured “no overuse injury in the past 6 months.” But the patient in front of you does have an injury. And she also sprained her ankle 3 months ago. So much for no injuries in the past 6 months…Real life is messy with lots of confounding variables. So this begs the question: are those studies even relevant to the patient in front of you?
3. Individual-based medicine
I’ve been quite lucky career. I have been in a situation where runners across the globe sought out my services to correct chronic imbalances and injuries, as well as search for performance limiters. Each one of these runners went through a robust musculoskeletal analysis, just as you likely perform with your patients. But every single runner I saw – over 7,000 of them! – also got a 3D research-grade biomechanical gait analysis utilizing almost 2 million dollars of equipment.
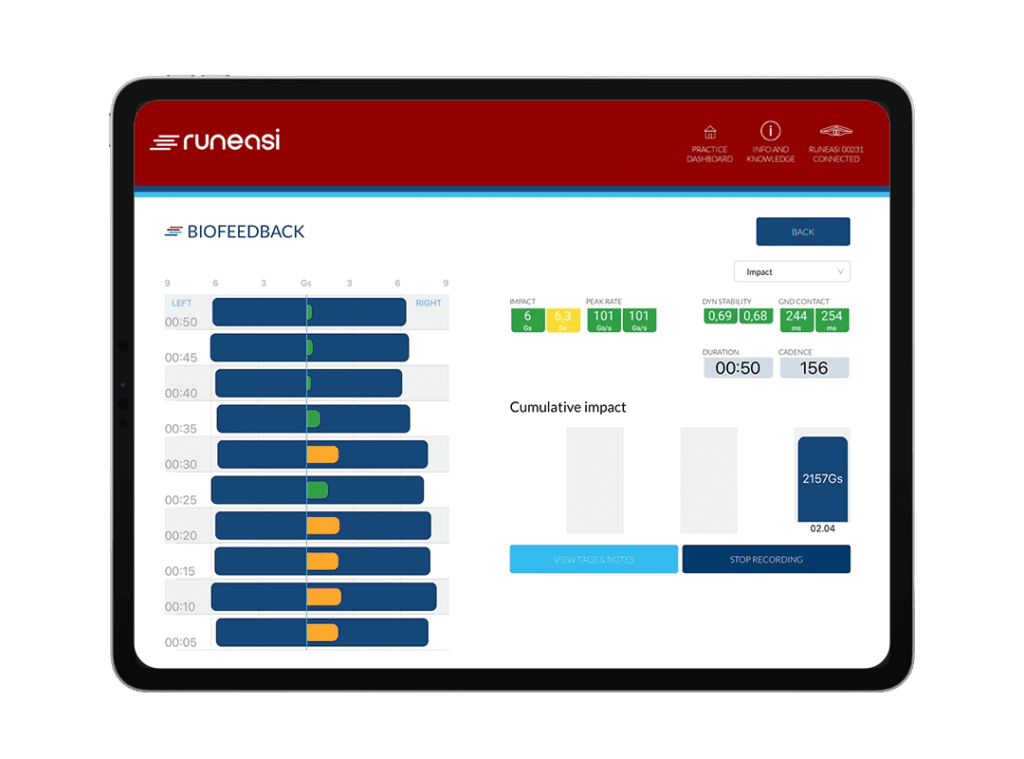
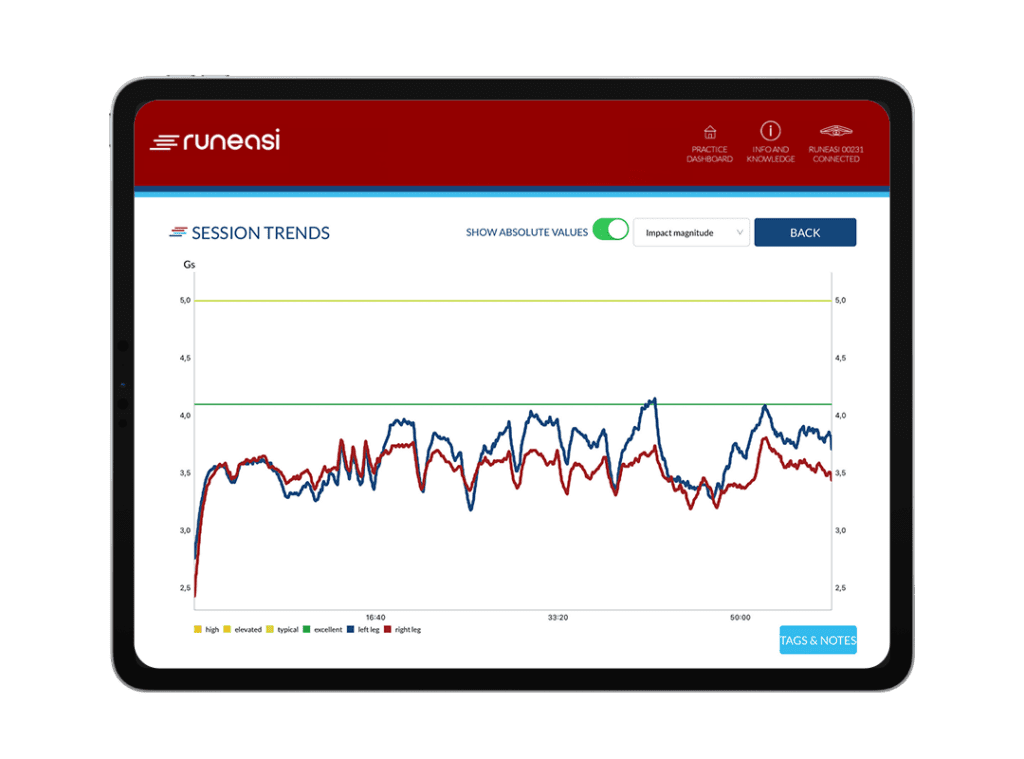
When you can assess their body, and their form, at a very high resolution, it actually becomes quite easy. The data helps you understand how their current level of mobility, stability, strength, and power manifests in their gait. It highlights the running form imbalances and symmetry. And after their evaluation, runners always have questions: how many times a week should I do this stuff? Can I run? If so how much? What cues should I think about when running?
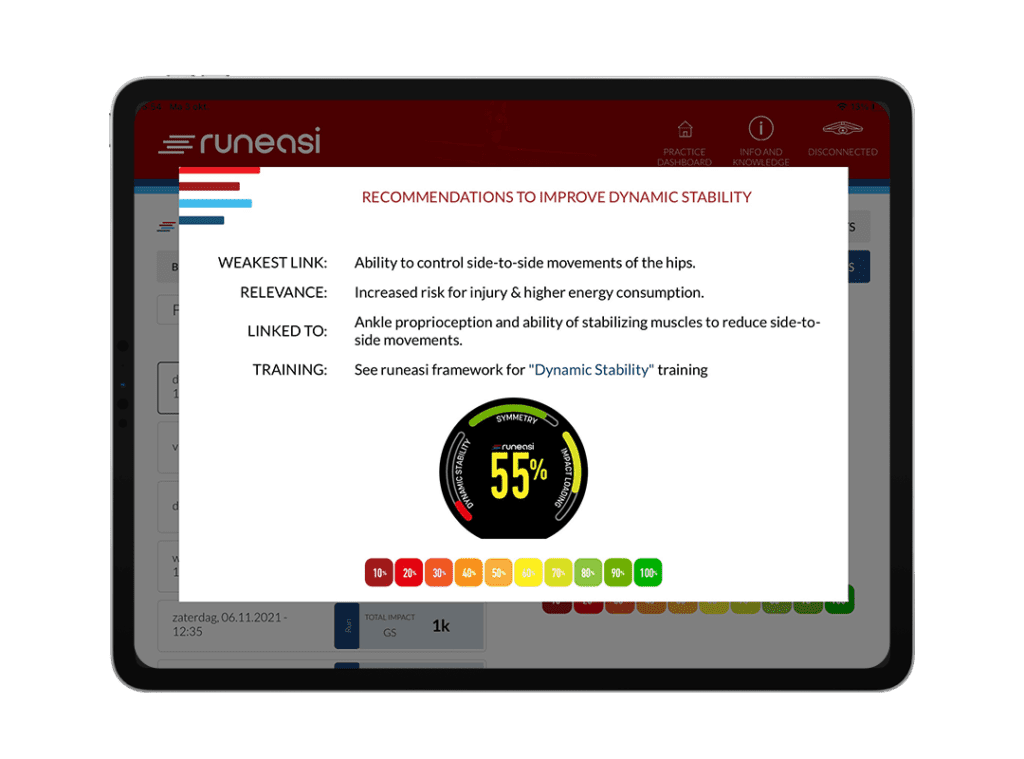
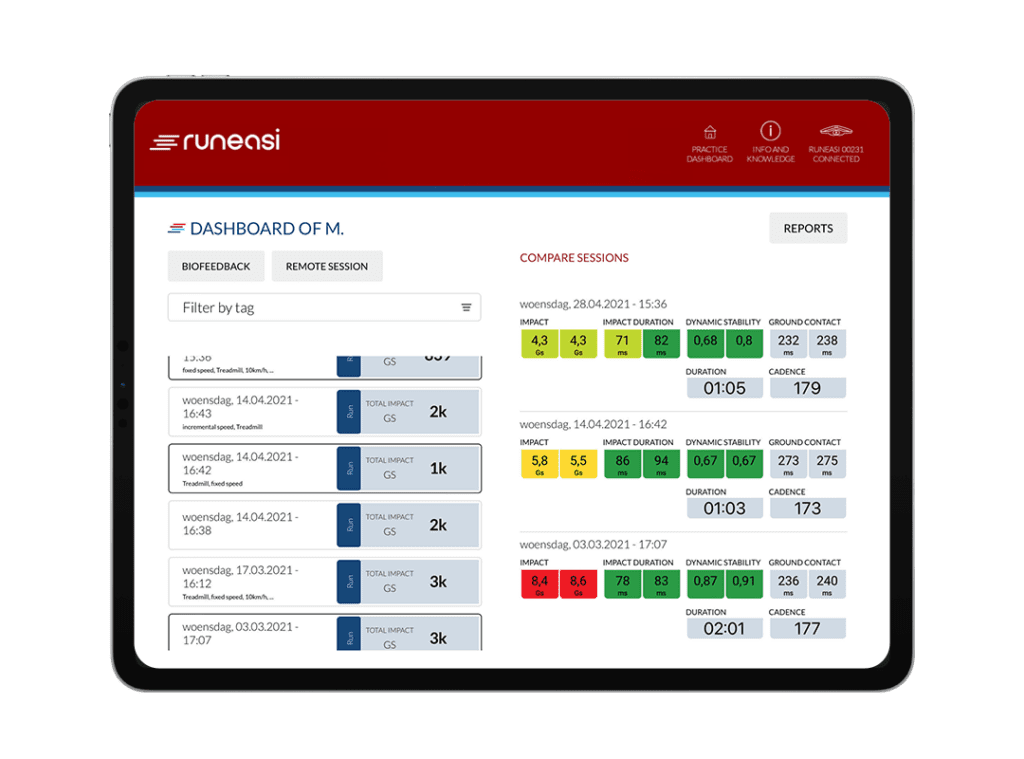
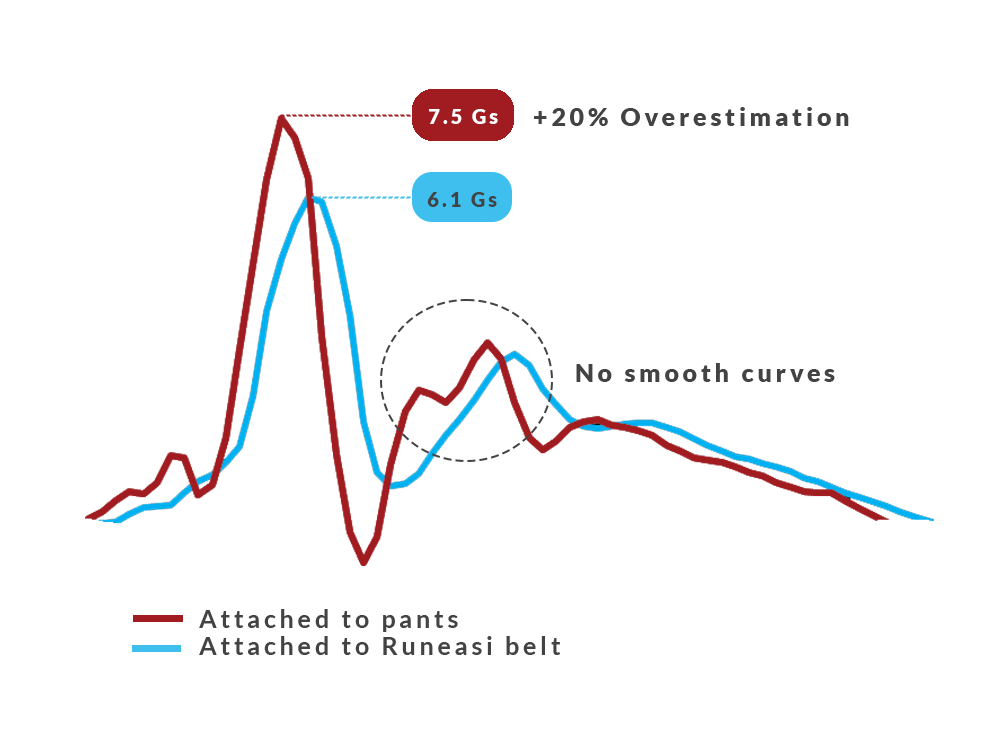
For most clinicians, we have to make educated guesses. But when you have high-resolution measurement tools, it takes the guesswork out of it. Each patient becomes a study of N=1. Individual research is much more specific than general research. These tools provide objective data points to help you decide exactly where to start for each individual, allow you to track their progress, and even call your own bluff.
Everyone has biases, and every runner is a unique person who responds differently to training and cueing. Having access to objective tools to assess runners removes the guesswork, and has been the single most powerful shift in my thought process and approach to runners. And I know it can be your hands as well.
"Objective data helps to push the needle in the right direction. If not, it's an insight to adjust the treatment course."
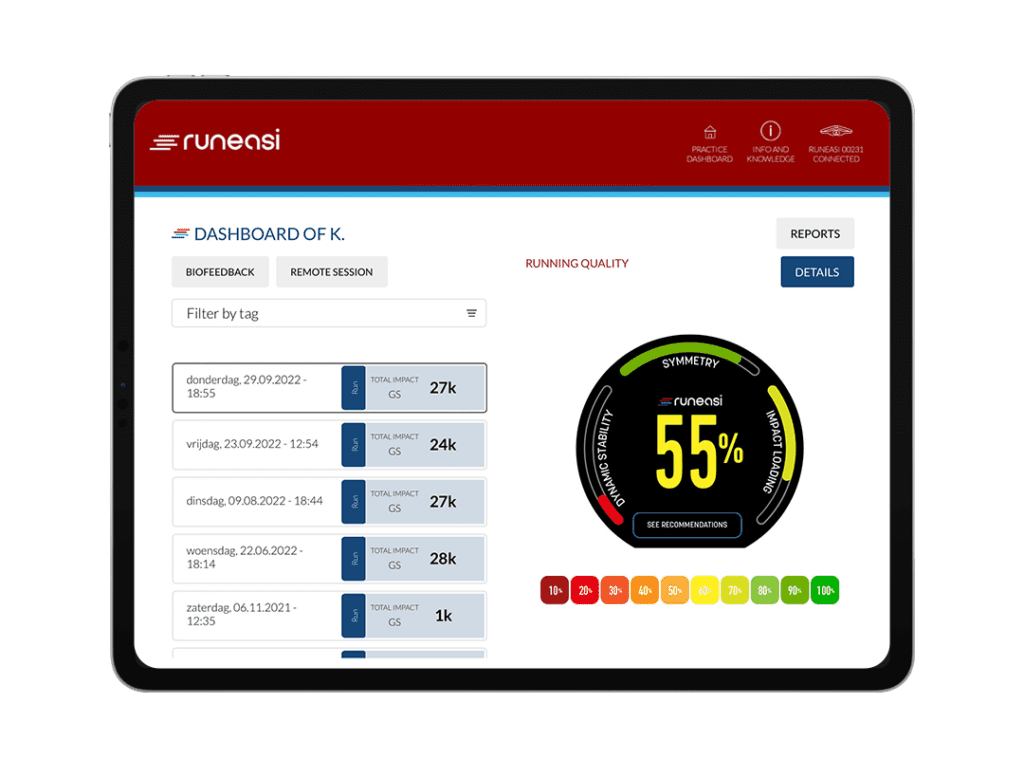
Technology advances are amazing. For decades we’ve lived in a time where you can get x-ray imaging, and see how bone heals. But we also live in a time where biomechanical assessment tools are making their way out of the lab and into the field. You can gather quantifiable data points from each individual runner, and ensure that the aims of your treatment are pushing the needle in the right direction for each runner you see. If you are on the right track you’ll measure improvements. If the needle moves in the wrong direction, you have objective insight to adjust your treatment approach.
"With RunEasi you’ll have a higher resolution lens to examine each one of your patients, and ensure they all hit their individual running goals."
I’m not discounting research. For good reason, our profession has made a commitment to incorporating research into our training to develop a solid foundation of critical thinking. But I always tell my students “research should guide your thought process, not tell you how to treat your patient in front of you.” With objective measurement tools like RunEasi, you’ll have a higher resolution lens to examine each one of your patients, and ensure they all hit their individual running goals.
Jay Dicharry, MPT, SCS
Oregon State University
Jay Dicharry, MPT, SCS,
Jay is a physical therapist, researcher, professor, and author who blends the fields of rehab and performance to optimize outcomes. He’s worked with over 50 Olympians, local standouts, and weekend warriors, and loves to see the smiles of his patients on top their own personal podium.
He has no financial ties to Runeasi.
4. Start incorporating individual-based medicine
Learn how to start measuring improvements in your patients and runners. We have many great case studies to discuss together over a free consultation with one of our RunEasi team members.